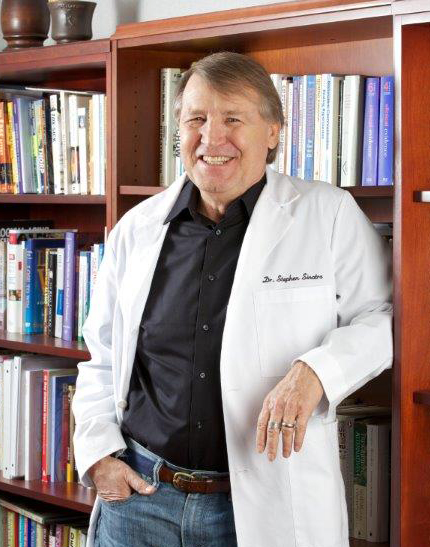
By Stephen T. Sinatra, M.D., F.A.C.C., F.A.C.N., C.N.S., C.B.T.
To say that I’ve been dealing with medication side effects for my entire career is no lie; within weeks of starting my cardiology practice, a hypertensive woman came to see me. She was reacting dramatically to a commonly prescribed diuretic and had developed a potassium deficiency that was causing muscle cramping and extreme weakness.
Even though I had prescribed drugs during my advanced medical training, I’d never seen a side effect that severe. It was an eye-opener, and the experience drove home the reality of adverse drug reactions. Textbooks and marketing ads generally describe medication side effects as “rare”—but they are real, and doctors too often tend to dismiss or downplay them when patients complain.
Too Many Meds
As my practice matured, I began to see more patients referred by internists and general practitioners in the area. Some of these folks were taking a half-dozen or more prescription drugs. Over time, a familiar pattern emerged. In addition to cardiovascular issues, these patients often had profound weakness and lethargy, disorientation, sleeplessness, nightmares, depression, heart failure symptoms (even when they didn’t have heart failure), constipation, and episodes of falling.
It became clear that drugs were exacerbating, rather than solving, their problems, and that these patients’ health was being damaged by the laundry lists of medications they were taking. Drugs for diabetes, hypertension, pain, depression, anxiety, cancer—you name it, they were on it.
I even had new patients who, as they were filling out medical history forms, asked for extra paper because six lines weren’t enough to write down all of their medications. One new patient was taking 18 drugs. It was medical madness!
The Rise of Polypharmacy and the “Polypill”
As you would expect, many of the patients I saw were elderly. With age, the body becomes less able to handle multiple medications and drugs are more likely to cause adverse reactions.
A 2015 report in the Journal of the American Medical Association calling out the dangers of “polypharmacy”—the prescription of five or more drugs to one person—gave me hope that this dangerous practice might change. But then I read an op ed piece in the Wall Street Journal advocating for a “polypill”—a single pill that contains medications for multiple conditions. For example, a statin may be combined with a blood sugar or blood pressure medication in a single tablet.
Heaven help us all.
Proponents of the polypill maintain that it will promote better patient compliance with taking medication and therefore improve outcomes. I see nothing but trouble. A polypill may make it more convenient for someone to take medications, but it doesn’t address the more fundamental issue—the fact that people are taking too many drugs in the first place. In fact, it just makes it easier to give them even more. That’s not smart medicine.
More Drugs, More Adverse Reactions
The biggest risk of polypharmacy is drug interactions. The more medications a patient takes, the higher the risk of unwanted or dangerous side effects. Here are some of the numbers:
- Nearly 50 percent of older adults take one or more medications that are not medically necessary.
- Interviews with 59 people over age 65 participating in one of Cuyahoga County, Ohio’s senior programs found that about 35 percent were taking five or more drugs. Of that 35 percent, more than half had contraindicated drug combinations. The same study revealed that polypharmacy was more highly associated with patients taking a drug more than once than with not taking a drug at all.
- Through a Scottish study of more than 300,000 patients of all ages, researchers found that the number of patients taking 5 or more drugs between 1995 and 2010 increased from 12 percent to 22 percent, and for 10 or more drugs from 1.9 to 5.8 percent. Among patients over age 65, 1 in 6 was taking 10 or more drugs.
- The estimated incidence of drug interactions rises from 6 percent in patients taking 2 medications a day to as high as 50 percent in patients taking 5 a day, according to one cardiology journal.
- A U.S. analysis showed that the proportion of outpatient consultations between 1995 and 2005 in which patients took 5 or more medications increased from 6 percent to 15 percent. The rate of outpatient or emergency room consultation where an adverse drug event was reported increased from 13 to 18 persons per 1,000 persons during the same period.
A Better Path to Health
The solution to this problem is clear to me. To reduce both the number of medicines prescribed and the risk of adverse drug reactions, it’s time for all doctors to fully embrace an integrative approach to medicine. Prescription medicines are one tool that can help patients get well. But alternatives such as dietary interventions, targeted nutritional supplements, and stress-reducing techniques can be just as effective—without the life-crushing side effects.
If you‘re on multiple medications, I urge you to have a heart-to-heart with your doctor about safely cutting down. Be direct; ask straight away if you truly need all those drugs. It may feel uncomfortable, but you have to be your own advocate.
In the meantime, there are steps you can take on your own to protect against medication side effects, and even lay the groundwork for getting off some of those drugs:
- Improve your diet. Follow an anti-inflammatory diet, like my Pan Asian Mediterranean Diet, which is full of antioxidant-rich fruits and vegetables. Antioxidant support is essential to help offset the inflammation associated with most chronic illnesses.
- Educate yourself about nutritional supplements. Consult with a nutritionally-oriented doctor who can customize a program of targeted supplements that provide extra “insurance” against nutrient-depleting drugs and inflammation.
- Minimize the sugar in your diet. Sugar may be the single most dangerous substance we eat in our food today, because it is a major cause of inflammation and metabolic disturbances. You simply cannot regain your health if your sugar consumption is high.
- Lose weight. For conditions such as high blood pressure or diabetes, a loss of just 5–10 pounds can make an enormous difference in the amount of medication needed to treat them. Remember, you may not be able to completely eliminate a drug, but you may be able to significantly cut down your dosage.
- Be active. Walking, dancing, or some form of regular physical activity—even a minimum amount—can make a difference in your health. It also will make losing weight easier.
- Get a handle on stress. If you take medication for anxiety, mild depression, or any other stress-related condition, try to reduce your dosage by exploring techniques that can help reduce your stress level. For additional support, I also like a homeopathic formula made from flowers called Rescue Remedy. It’s definitely worth keeping handy for occasions when you feel anxious or stressed.
- Support your liver. This organ processes the medications you’re taking and detoxes them out of your system, which means it’s extremely important to keep it working efficiently. Buildup from too many meds can lead you down a path toward liver failure. You can help your liver by eating artichokes a couple times a week and taking the nutritional supplement milk thistle. Both are high in compounds that protect the liver.
- Get (and stay) grounded. Last but not least, use Earthing to reconnect your body with the natural energy in the ground. Research is showing that grounding can reduce inflammation and inflammatory symptoms such as pain, as well as improve sleep and energy.
Taking these steps not only will help you protect yourself from drug toxicity and adverse reactions, but improve your health enough that you may not need so many medicines to begin with. Even a reduction is a win. If you can take three or four drugs instead of five—or even more—you’re better off.
References:
- Scott IA, Hilmer SN, Reeve E. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-34.
- Lin, P. Drug interactions: A method to the madness. Perspectives In Cardiology. 2004;20(10):20.
- Guthrie B, et al. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Medicine. 2015;13:74.
- Bourgeois FT, et al. Adverse drug events in the outpatient setting: an 11-year national analysis. Pharmacoepidemiology and Drug Safety. 2010;19(9):901-10.
- Pereira A, et al. Infusions of artichoke and milk thistle represent a good source of phenolic acids and flavonoids. Food Funct. 2015;6(1):56-62.
- Konner M. A ‘polypill’ may be the next big preventative fix. Wall Street Journal. 8 Jun 2016.
- Maher RL Jr et al. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014 Jan;13(1):10.
- Golchin N et al. Polypharmacy in the elderly. J Res Pharm Pract. 2015 Apr-Jun;4(2):85–88.
© 2015, 2016 HeartMD Institute. All rights reserved.