By Stephen T. Sinatra, M.D., F.A.C.C., F.A.C.N., C.N.S., C.B.T.
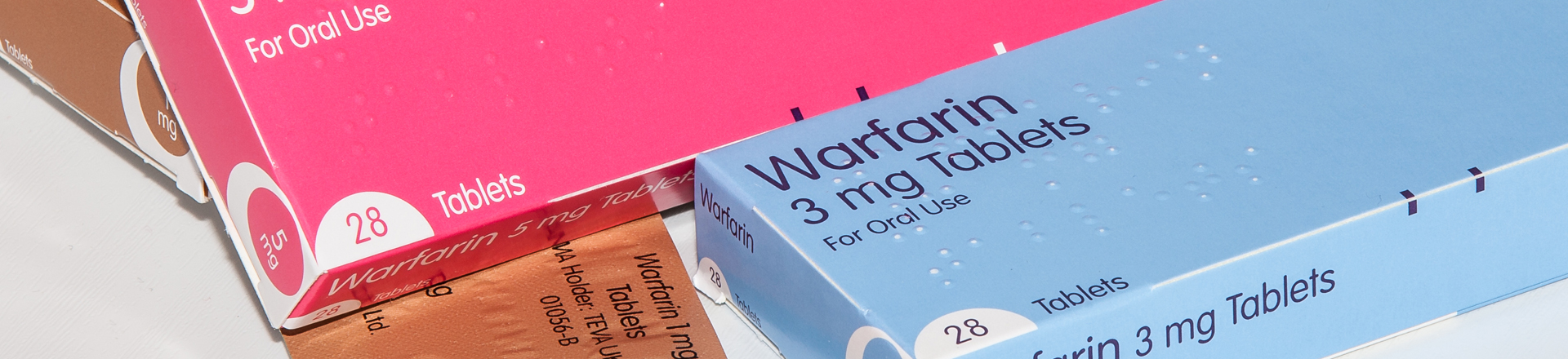
Patients taking Coumadin (warfarin) often ask, “How can I get off this drug? Are there any natural alternatives that would work just as well?” Many are tired of the inconvenience and discomfort associated with having blood drawn every 4-6 weeks to monitor the drug’s anticoagulant action, or may worry about the risk of abnormal bleeding. Some detest experiencing unpleasant side effects like weakness and abdominal discomfort, and others simply don’t like the nature of warfarin (it’s used as rat poison in large quantities).
Despite all the negative aspects of Coumadin use, there’s a reason it is so widely prescribed… With an unparalleled ability to thin the blood and prevent blood clotting, it has a fantastic track record of protecting against stroke. A stroke is death of brain tissue caused by the lodging of a blood clot, or fragment of one, in an artery and subsequent prevention of blood flow to the brain. Hence, while there are some people on Coumadin who may benefit from switching to natural alternatives, certain higher-risk individuals really need to stay on it to prevent strokes.
Who Should Stay on Coumadin?
As of yet, there aren’t any blind studies which demonstrate that any natural alternative is as effective against stroke as Coumadin; Coumadin is the best preventative option for patients who are likely to experience blood clotting or stroke related to clot displacement. In general (without knowing a person’s medical or family history), staying on Coumadin is often recommended for people who have:
- Hearts with enlarged chambers or valves that do not function properly;
- Had an extensive heart attack; the resulting scar tissue can weaken the left ventricle and allow blood to clot more easily;
- Prosthetic or mechanic heart valves, or a pacemaker; blood is more likely to stick to the artificial surfaces;
- Endured an embolic stroke (one of three kinds of strokes, where a fragment or clot of blood pumps from the heart to the brain); or
- Atrial fibrillation, where atria don’t contract; blood can form pools and become sluggish.
The one exception here is patients with “lone” AF… Patients who have had AF occur only once or twice and have an otherwise healthy heart – of normal size, and without enlarged chambers or leaky valves – may be candidates for more natural Coumadin alternatives as long as they are not otherwise prone to blood clots or other heart risk factors like diabetes.
Coumadin Alternatives
A person taking Coumadin, who is not in any of the abovementioned situations, may want to try more natural blood thinning alternatives, such as:
- Nattokinase – an enzyme extracted and purified from natto, a traditional Japanese soybean dish. Nattokinase is a good supplement to take to help thin the blood. It helps prevent blood clots by reinforcing the actions of plasmin, an enzyme in the body that breaks down fibrin – 100 mg daily;
- Fish Oil – 2-3 grams daily;
- Garlic – 1-2 grams daily in capsule form, or as much raw garlic as you can tolerate;
- Vitamin E (as mixed tocopherols) – 100 – 200 IU daily;
- Bromelain (an enzyme derived from pineapple) – 600 mg daily;
- Aspirin– As an anti-platelet agent, aspirin also has anti-clotting properties, and is frequently prescribed to help manage cardiovascular disease. While aspirin is also used to prevent ischemic strokes, it is less effective than Coumadin for preventing clots and strokes. It can also increase risk of hemorrhagic stroke (triggered by a leaky blood vessel in the brain);
- Grounding– connecting to the Earth’s electromagnetic energy has been shown to help improve zeta potential, the tendency for red blood cells to repel one another. Grounding is also cardio-protective in that it can support heart rate variability and can help reduce stress by relaxing the body (as shown through increased parasympathetic nervous system activity).
If you take Coumadin, it is extremely important to consult with your prescribing physician if you are considering adding natural blood thinners to your program; hopefully s/he is holistically-minded and has knowledge of natural medicines (if not, bring him or her literature about them). It can be dangerous to mix Coumadin with natural alternatives because excessive bleeding can occur; this is especially problematic for people over the age of 85 because they are at higher risk of hemorrhagic stroke. Stopping Coumadin use entirely can also dramatically change blood viscosity, so be sure to discuss potential risks and benefits of all courses of action with your physician if you are considering natural alternatives.
Other Coumadin Concerns
Vitamin K2 is a Coumadin antagonist, which means it can limit Coumadin’s blood thinning capability. However, K2 plays an important role in cardiovascular health. It helps get calcium into bones instead of letting the mineral build up in arterial walls, which can cause arteriosclerosis. It’s important then, for people on Coumadin to abstain from vitamin K2 supplementation, and to instead eat leafy green vegetables and/or cheese, which contain vitamin K1 and K2, to avoid deficiency…. The key is moderation.
The same reasoning applies to grounding. While people on Coumadin may stand to benefit from standing barefoot outdoors for an hour or so each day, utilizing a grounding device for many hours a day or overnight is not recommended because of risk of excessive bleeding. People who wish to ground to improve their quality of life must work with their physician and get tested regularly to determine the thickness of their blood.
Note: Coumadin (warfarin) is the most commonly prescribed oral blood thinning agent; other blood thinners that doctors may use include Heparin, Lovenox (enoxaparin sodium), Normiflo (ardeparin sodium), and Orgaran (danaparoid sodium).
© 2011, 2014 HeartMD Institute. All rights reserved.